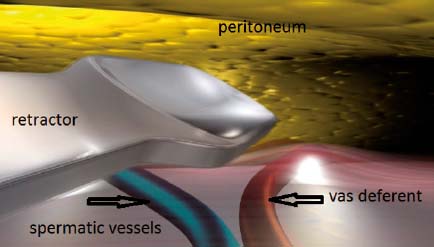
Fig. 10.1
Specific retractor

Fig. 10.2
MOPP incision
10.2 10.2 Prosthesis and Instrumentation
The prosthesis is selected according to the need to be unrolled in the preperitoneal space, through a small incision. A wide polypropylene mesh prosthesis has been specifically devised for this technique; it has a peripheral hem with a reinforcement (Fig. 10.3) to facilitate proper deployment of the prosthesis. The prosthesis is available in two sizes, 16.5 cm/12 cm and 13.5 cm/9 cm. The quality of the prosthesis allows for the minimally invasive technique. This technique requires some very long and narrow retractors (Fig. 10.1) allowing a wide and deep dissection. A long dressing forceps with an atraumatic end is used to introduce the prosthesis behind the pubic bone, in contact with the bladder, without any risk of causing injury to it.
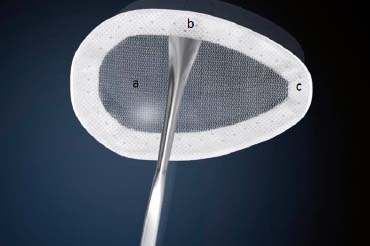
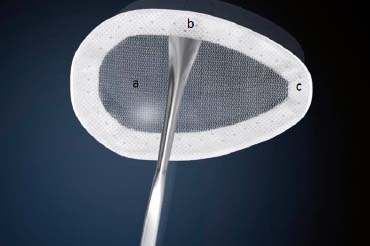
Fig. 10.3
The MOPP prosthesis. a Large pore size polypropylene mesh. b Non-knitted non-woven peripheral reinforcement. c Peripheral hem
10.3 10.3 Surgical Technique
10.3.1 10.3.1 The Minimal Open Route Between the Skin and the Deep Inguinal Ring
The skin incision (Fig. 10.2) is deliberately small. With experience it can be between 25 and 40 mm. It lies immediately in front of the deep inguinal ring. Several landmarks can be drawn on the patient’s skin. The easiest approach is to simply connect the superior anterior iliac spine to the pubic tubercle and draw the incision transversely to the union of the internal and middle third.
After incision of the skin and subcutaneous layers, the fascia of the external oblique muscle is incised in line with its fibers. The ilioinguinal nerve is generally identified and preserved.
The spermatic cord is dissected (Fig. 10.4), separating the funicular pedicle (the blue line) which is left behind. Time to time it is necessary to separate an old and fibrous medial sac from the spermatic cord. The cord is also separating from the ilio inguinal nerve. I never cut the cremaster fibers: they are retracted medially. At this step, a lateral hernia sac is sought: locating a large and old sac is easy, but sometimes you find a small sac in the most proximal part of the cord. The lateral sac is separated from the cord (Fig. 10.5). Similarly, a lipoma of the cord will also be dissected and resected, as its persistence may be responsible for postoperative pain, sometimes feeling like a pseudo recurrence. Parietalization of the sac is initiated, pushing it through the deep inguinal orifice.


Fig. 10.4
Externalization of the spermatic cord
10.3.2 10.3.2 Cleavage of the Preperitoneal Space
Penetration into the peritoneal space starts through the deep inguinal ring, laterally to the epigastric vessels, previously identified (Fig. 10.6). Cleavage of the preperitoneal space is initiated (Fig. 10.7), back to the transversalis fascia — which is very fine at this location — pushing it medially and progressing back to the inferior epigastric vessels; the vessels are pressed against the anterior abdominal wall, where they will be well protected throughout the procedure with a retractor. Using the dedicated retractors (Fig. 10.8), the dissection extends into the avascular plane medially and laterally along the inferior epigastric vessels in the direction of the iliac vessels, quickly and easily, cleaving the spaces of Retzius and Bogros. Cooper’s ligament is easily spotted, the bladder pushed back, and the retropubic space is cleared (Fig. 10.9). Dissection of the space for accommodating the prosthesis continues inwards and upwards with retractors of increasing size. Facing the upper edge of the incision, the peritoneum may be more adherent to the superficial plane and must be gradually separated with scissors; it is imperative to widely open the plane at this level. The top and posterior dissection is easier to widely explore the psoas muscle.



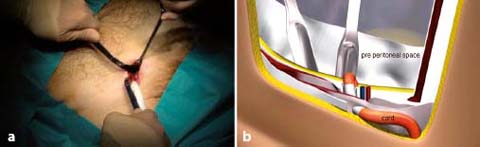
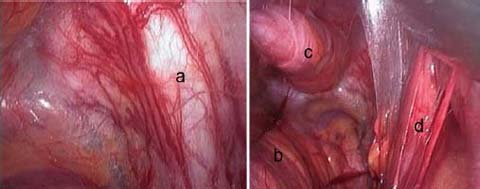

Fig. 10.5
Individualization of the lateral hernia sac

Fig. 10.6
Inferior epigastric vessels identified

Fig. 10.7
Cleavage of the preperitoneal space is initiated through the deep inguinal ring
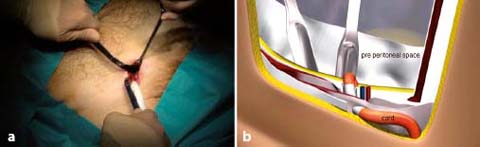
Fig. 10.8
a Dissection of the preperitoneal space with the specific retractors. b Dissection of the preperitoneal space with the specific retractors, synthetic image
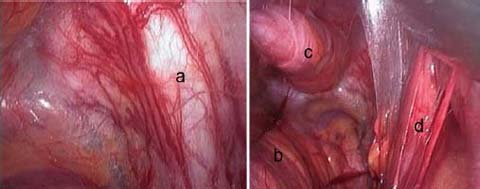
Fig. 10.9
Dissected preperitoneal space. a Cooper’s ligament. b Bladder. c Visceral sac. d Spermatic cord with a large lateral sac
10.3.3 10.3.3 Parietalization of the Spermatic Cord
The elements of the spermatic cord should be separated from the peritoneum, about 10 cm relative to the deep inguinal ring, so as to achieve parietalization of the cord (Fig. 10.10). During the dissection, the spermatic sheet described by R. Stoppa [7], uniting the vas deferens medially and the spermatic vessels laterally, must be carefully respected, if possible. After parietalization, this spermatic fascia can be interposed between the prosthesis and the external iliac vessels. After dissection of the cord, the “parietalization triangle”, of which the summit is the spermatic cord, the medial edge the vas deferens, and the lateral edge the spermatic vessels, is well exposed (Fig. 10.11).